The Situation: Promised Pharmacy Savings Hinged on Income Level
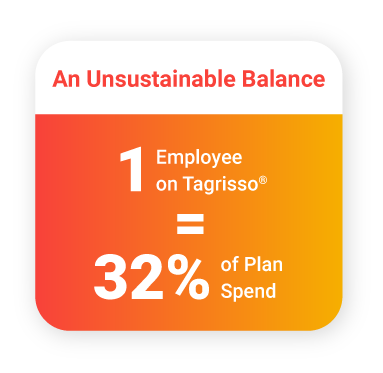
With 500 employees and their families on a half-million-dollar plan, one self-funded trucking company needed to better balance their benefits budget with the unique needs of those who depend on them for healthcare. Their benefit advisor recommended a plan swap that would use a patient assistance program, but a missed condition in the contract kept them from seeing the savings they were promised – the member on an expensive specialty drug could never receive the promised dollars because of their income level. This unforeseen roadblock left the company on the hook for the cost of the specialty drug and put their entire plan at risk.
The Solution: Expert Claims Review Recovers Lost Savings
The company’s priority became finding a better pharmacy benefit partner. The company and their benefit advisor engaged RxBenefits for an expert pharmacy claims review, and the resulting analysis found more than cost reductions for the expensive specialty drug. Experts found the plan could save $27K annually on Tagrisso®, and the review uncovered off-label prescribing of diabetes medication for weight loss accounting for another 22% of the plan’s cost.
The Impact: Continuing to Reduce Wasteful Spending and Improve Employee Health
By using actual member data, the program is protected against further wasteful pharmacy spending, from high-cost treatments to off-label prescribing. In addition, the plan is designed to handle the unique specialty medication challenge of Tagrisso® by using ExpressScripts’ SaveOnSP program. Employees and the company both have an extra layer of protection to ensure medical necessity, member safety, and cost effectiveness in their pharmacy benefit. As the company’s employee base continues to grow, change, or face new diagnoses, the RxBenefits clinical management program will continue to offer the best benefit with lowest net cost.

Contact your benefit advisor to learn more.

