
Embrace, Adapt, Succeed:
What Every HR Leader
Should Know About Disruption
From formulary changes to
prior authorizations, when to
embrace change
HR leaders may fear pharmacy benefit disruption will take their employees out of their comfort zone and create more headaches than growth opportunities. But in reality, members experience disruption regularly, and with an expert member and plan advocate on your side, you can minimize friction when making a benefits change.
Minimal Disruption Can Maximize Savings
Fundamental Disruption: Formulary Changes
PBMs change formularies regularly – often, multiple times per year. Members may need to switch to an equally effective alternative medication based on these changes, which shows employees can handle changes when they need to.
Ensure Your Plan Meets Expectations
Basic utilization management techniques like prior authorizations and step therapy protect member health and plan sponsors’ dollars and ensure the pharmacy plan meets the business’s expectations.
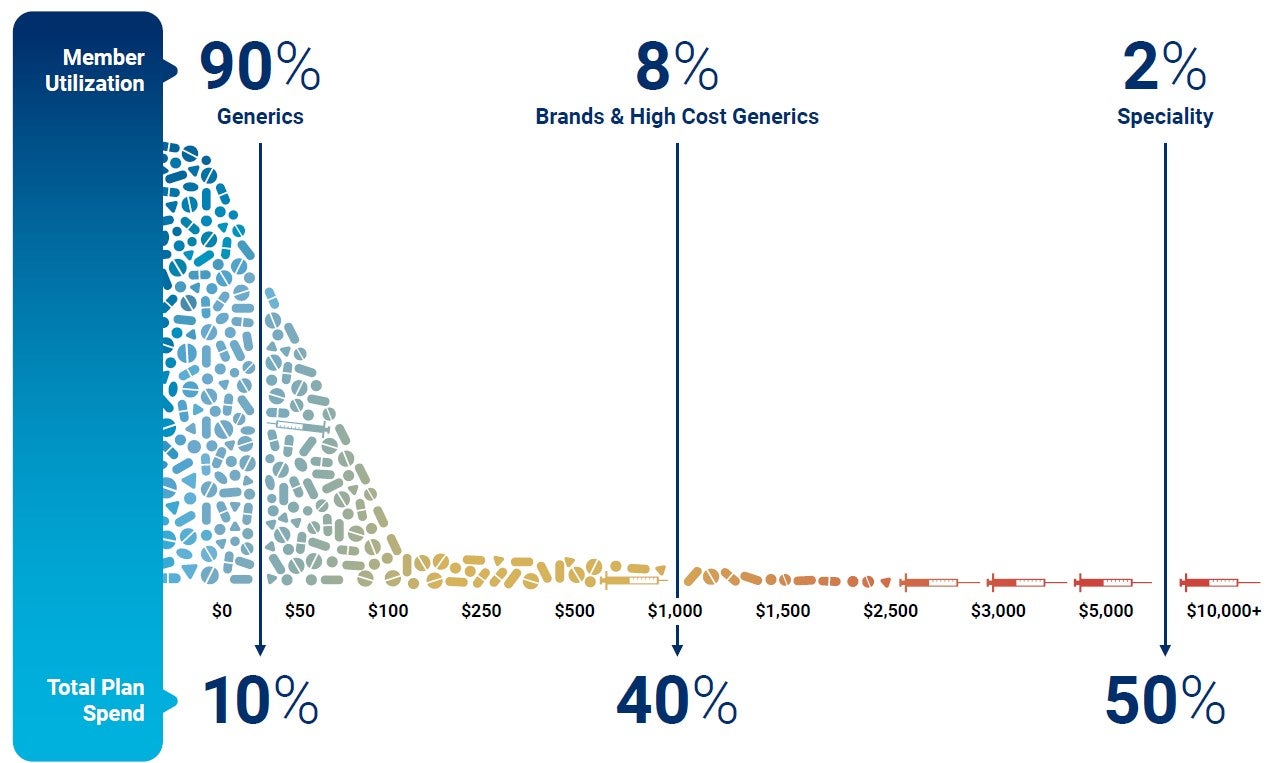
Focus on the Most Severe Conditions
On average, only 2% of members use the most expensive specialty drugs and need the most care and attention. They drive 50% of pharmacy plan costs. A deep knowledge of members, specialty
medication trends, and the changes that will impact costs while minimizing unnecessary disruption is needed to create successful UM programs.

Ensure your members get the treatments they need —
without paying for unnecessary, high-cost drugs.
