Healthcare costs are skyrocketing, and self-insured employers find themselves in a daunting predicament: striving to deliver optimal health benefits to their employees without breaking the bank. A survey from the Kaiser Family Foundation shows 87% of employers believe offering health benefits will become too expensive within the next five to 10 years.
In 2023, it’s crucial for employers to understand what’s happening in the pharmacy benefits market and how to face its challenges head-on while maintaining an overall attractive benefits package. Our on-demand webinar, RxBenefits Innovation 2023, tackles these challenges and provides key insights and recommendations for self-insured employers to stay ahead of the tsunami of specialty costs.
These key insights from the webinar will help you navigate the pharmacy benefit world in Q3 2023.
Watch the webinar RxBenefits Innovation 2023
Diabetes medicines drive high pharmacy costs for employers
Diabetes medicines are a large driver behind the mounting pharmacy costs for employers, making up 18% of the total costs for RxBenefits’ self-insured customers in 2022.1 As the number of people with Type 2 diabetes in the United States keeps going up, so does the cost of medications used to treat the condition.
The allure of celebrity endorsements and the influence of social media trends have propelled the popularity of certain diabetes drugs, such as Ozempic and Mounjaro, for weight loss purposes. The off-label use of GLP-1 diabetes drugs drives about 40% of plan spending in this category, and Ozempic stands out as a significant contributor.1
Biosimilars have potential for cost reduction but face limitations
Will 2023 be the year of biosimilars? Biosimilars have the potential to bring down costs. But so far, their impact remains limited due to a strict approval process, supply challenges, and limited interchangeability with the original drugs.
The FDA has approved eight biosimilars for Humira, a widely used drug for rheumatoid arthritis, introducing increased competition to the market, with a biosimilar interchangeable for Humira scheduled for release in July. With 27% of plan costs for self-insured employers coming from anti-inflammatory medications and dermatological agents, self-insured plan sponsors need relief from these drug categories.1
Protecting your organization with supplemental stop-loss coverage
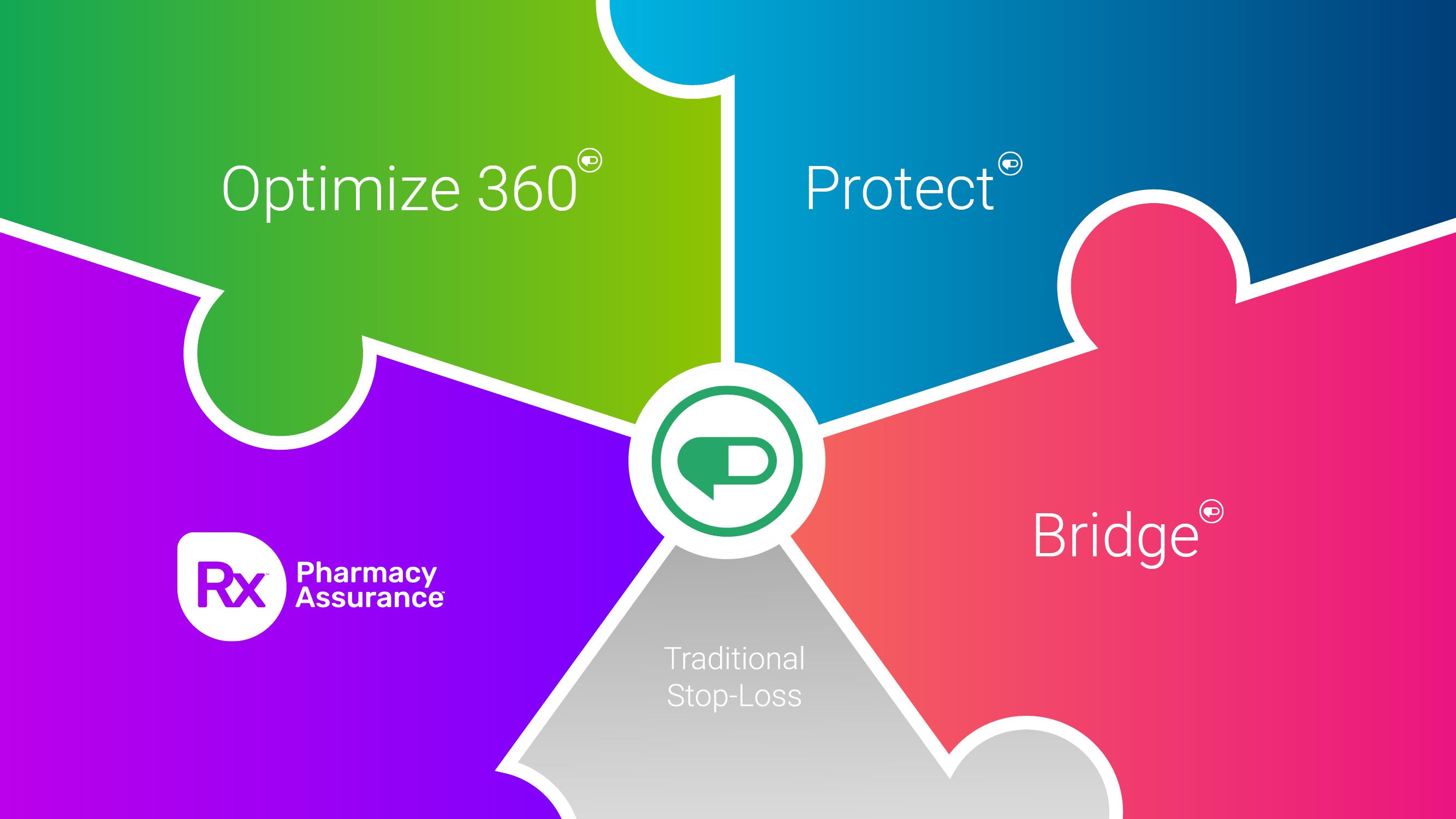
Regular stop-loss coverage helps with unexpected medical and pharmacy claims, but it might not cover ongoing treatment for chronic conditions. To shield yourself from the rising costs of specialty medications, you need strong supplemental stop-loss coverage.
Tailored supplemental stop-loss coverage for pharmacy claims can bridge that gap and give you comprehensive protection against sudden cost increases.
Learn about affordable supplemental stop-loss for specialty medication claims.
Create tailored pharmacy benefit solutions that fit your organization’s needs
At RxBenefits, we understand the growing challenges faced by self-funded employers in the ever-changing pharmacy landscape. That’s why our tailored pharmacy benefit solutions are designed to fit the unique needs of your organization and its employees.
Just like a skilled rock climber knows the importance of layered protection, we recognize the need to mitigate risks faced by your organization. If you’re concerned about providing employees with essential medications without one large specialty claim breaking the bank, you’re not alone.
Our innovative and responsive solutions are designed to address the current challenges employers face while preparing for the future. We are committed to ongoing innovation to deliver targeted enhancements and all-new solutions that tackle present and future obstacles.
You are the expert for your organization, serving the needs of your employees and earning their loyalty. As your partner, we provide the innovative solutions necessary to support your efforts and ensure the best outcomes for your employees.