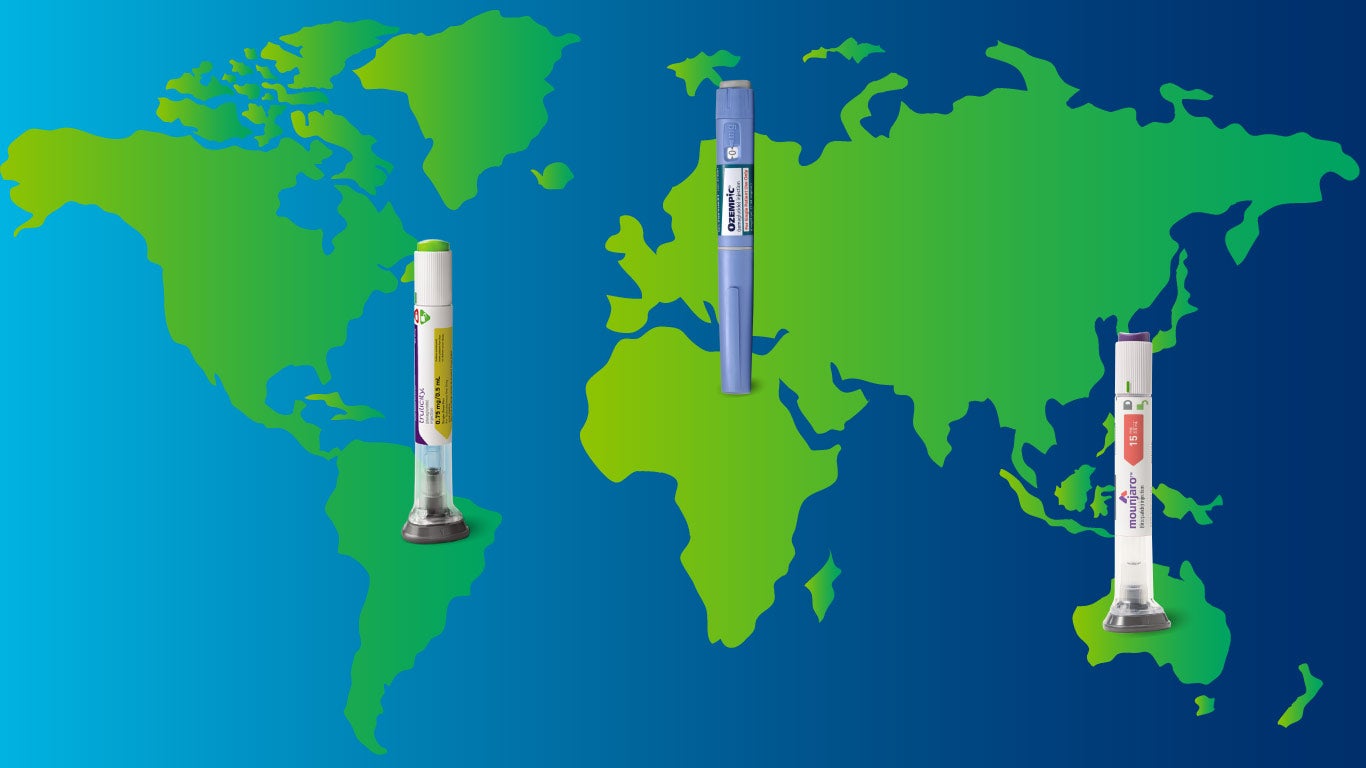
Driven by factors like social media, shrinking celebrities, and the broader availability of telemedicine, GLP-1 drugs such as Ozempic®, Trulicity®, and Mounjaro™ have proved to be more than a passing fad. The drugs, originally developed to treat type 2 diabetes, were successful at helping patients with the condition manage their blood sugar levels – with a side effect of causing significant weight loss. That has led to explosive growth in off-label prescribing, as well as the increased popularity of GLP-1s such as Saxenda® and Wegovy® approved for weight-loss purposes.
This growth has been particularly hard on self-funded plan sponsors. Prescribed on-label or off-label, for type 2 diabetes or for weight loss, GLP-1s are expensive – from $750 to over $1,000 for a 30-day supply. That can make it tempting for plan sponsors and members to look for cheaper options, such as sourcing the drugs internationally rather than purchasing the drugs through their pharmacy plan.
At first glance, importing a drug from Canada, Mexico, or Europe for as little as a quarter of the price can seem like an easy choice for plan sponsors and members. How can they lose by saving money? However, even if the price tag is low, the ultimate cost can be high.
Sourcing internationally means forgoing protection.
Purchasing any drug outside the U.S. carries risks. One of those risks is legal – current FDA guidance bars patients from importing drugs into the U.S. with only two exceptions: if the drug isn’t used to treat a serious condition and presents no known significant health risk, or if an effective treatment for a serious condition isn’t available in the U.S. The second exception is subject to several additional requirements outlined in FDA guidance on personal importation. Adherence to either of those conditions is questionable in the case of GLP-1s.
While a recent FDA ruling approved some mass drug importation from Canada, the ruling is limited in scope – impacting only state plans in Florida – and currently facing pushback from drug manufacturers and from the Canadian government, which blocks export of prescription drugs that are in short supply – like many GLP-1s.
A greater risk is the danger to the patient’s health. The FDA has put numerous safety mechanisms in place to protect consumers from negative outcomes from their medications. Even if the drug is purchased from a vendor in a well-regulated country like Canada or the U.K., there’s no guarantee as to where the vendor is sourcing its medications. The FDA has outlined stringent standards for entities all along the supply chain to ensure the medications a member obtains in the U.S. are safe, properly labeled, and as described.
This has become a particularly significant concern as demand for GLP-1s has caused a worldwide surge in counterfeit versions. Counterfeit GLP-1s have been found in over a dozen countries, with many patients hospitalized after taking them. Consumers have no way of knowing what’s actually in the product they purchased overseas.
Plan sponsors and members purchasing drugs outside of the U.S. are also forgoing another crucial layer of protection: clinical oversight. When a medication is filled through their PBM, a clinical pharmacist with access to utilization data can review the prescription to ensure it’s been appropriately prescribed and won’t negatively interact with any of the member’s other medications. The pharmacist can also determine if a less expensive drug could be as effective as the one prescribed, saving the plan sponsor from wasteful spending while protecting the member.
Sourcing domestically can protect lives and bottom lines.
Avoiding the risks and dangers associated with international GLP-1 sourcing doesn’t have to result in budget-breaking expenses for plan sponsors. Utilization management is key to offsetting the cost of pricey drugs like GLP-1s. RxBenefits’ clinical management solution, Protect, offers prior authorization enhancements to prevent off-label prescribing of type 2 diabetes drugs by confirming a diagnosis before approving the claim.
Plan sponsors can limit their spend on GLP-1s by choosing to exclude weight-loss drugs entirely from their coverage, or prevent unnecessary expenses with utilization management rules. Many plan sponsors concerned with the four-figure price tags for some GLP-1s are still willing to cover other weight-management programs, particularly those that address behavioral and lifestyle modification. Members whose weight-loss drugs aren’t covered by their employer’s plan can look to manufacturer assistance programs to help them cover the cost.
While the promise of low-priced drugs purchased overseas can be attractive, plan sponsors should be aware of the risks they’re facing – and the alternatives available. With rebates, manufacturer assistance dollars, and proper utilization management solutions in place, a plan sponsor may well be able to beat the price of an international vendor by a significant amount. And they can take comfort in knowing the members’ medications are safe and properly prescribed.





